Subclinical hypothyroidism
- related: Endocrine, Elderly patients have higher TSH concentration, hypothyroidism
- tags: #note
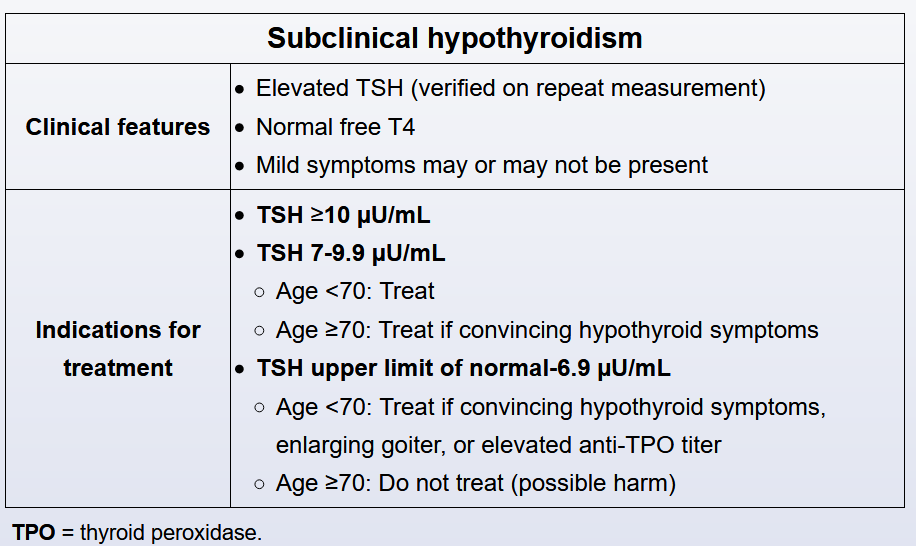
Subclinical hypothyroidism (SCH) is defined as an elevated serum TSH level with a normal free thyroxine. The most common cause is chronic lymphocytic Hashimoto thyroiditis. The decision to treat SCH with levothyroxine depends on the magnitude of TSH elevation, age, presence of goiter, and whether there are symptoms definitely attributable to hypothyroidism. In addition, high circulating levels of anti-thyroid peroxidase (anti-TPO) antibodies (seen in >90% of patients with Hashimoto thyroiditis) are associated with progression to overt hypothyroidism and can identify patients who are likely to benefit from treatment.
This patient has a mild TSH elevation and nonspecific symptoms (eg, fatigue, weight loss followed by weight gain), some of which could be attributable to medications (eg, topiramate). Measuring the level of anti-TPO antibodies would help establish the diagnosis of Hashimoto thyroiditis and facilitate management decisions
Subclinical hypothyroidism is associated with an increased risk for a number of pregnancy complications, including recurrent miscarriages, severe preeclampsia, preterm birth, low birth weight, and placental abruption. In addition, anti-thyroid peroxidase (anti-TPO) antibodies are associated with increased risk for pregnancy loss, even in women who are biochemically euthyroid. Treatment of subclinical hypothyroidism associated with high titers of anti-TPO antibodies may reduce the risk of recurrent miscarriages.
This patient has subclinical hypothyroidism, defined as a serum TSH above the upper limit of normal with serum free T4 in the normal range. Subclinical hypothyroidism is often associated with symptoms that suggest a hypothyroid state, but in most cases symptoms are vague and highly nonspecific (eg, fatigue, constipation). Treatment of subclinical hypothyroidism is recommended for all patients with TSH ≥10 or those age <70 with convincing hypothyroid symptoms or features associated with progression to overt hypothyroidism (eg, enlarging goiter, elevated anti-thyroid peroxidase antibody titer).
In contrast, older (age ≥70) patients with subclinical hypothyroidism warrant more conservative management. Levothyroxine replacement in this population confers less benefit than in younger patients and carries an increased risk for adverse events (eg, atrial fibrillation). In addition, some experts believe that the true normal TSH range in older patients may be higher than in younger patients, and levels as high as 8 µU/mL may represent physiologic euthyroidism in patients age >80. In lieu of treatment, older patients should be monitored with periodic retesting (eg, in 1-3 months and every 6-12 months thereafter), and treatment should be considered for those who progress to overt hypothyroidism (Choice A).